Don’t Live with Back Pain, Learn about Cervical Stenosis
It is the narrowing in one or more areas of the spine due to injury or deterioration of the discs, joints or bones within the spinal canal. There are two main types of this condition:
Lumbar Spinal Stenosis – This condition affects the lower back and lumbar area. Its symptoms will often be felt in the lower back, buttocks, and legs
Cervical Stenosis – This condition affects the neck and cervical spine. Its symptoms will often be felt in the neck, shoulders, and arms
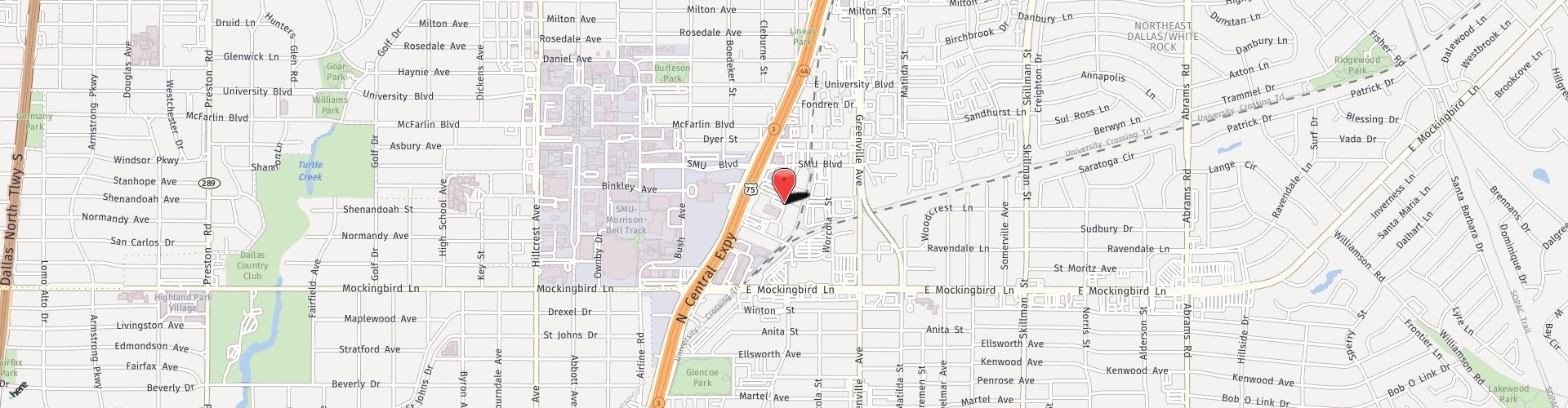
If you think you have cervical stenosis, contact our offices in Dallas, TX to learn more.

Patient Testimonial
“Dr Barnet and all of his staff, especially Lana, went above and beyond to make my surgical outcome a success with the minimum amount of inconvenience. the surgery was successful and I am pain-free and feel better than I have in many years. I am very grateful to have had such a great experience and outcome my surgery was a complete and total success. Thank you Dr. Barnett.” – Diane Tasma
What is Foraminal Stenosis?
A subtype of spinal stenosis is foraminal stenosis. This condition is caused by a narrowing of the foramen, the opening within each of the spinal bones that allow nerve roots to pass through. As a result of aging or other musculoskeletal conditions such as arthritis, the foramen may gradually develop bone spurs that can press on the nerves, causing pain and other symptoms.
Patients with this condition may experience numbness, weakness, and tingling sensations throughout the arms and legs, depending on which area of the spine is affected.
Effective treatment of foraminal stenosis can usually be achieved through nonsurgical techniques including anti-inflammatory medications, corticosteroid shots, physical therapy exercises or wearing a brace. Those patients whose conditions do not respond may require a surgical procedure called foraminotomy.
What aggravates Cervical Spinal Stenosis?
Cervical spinal stenosis presents symptoms because one or more of the nerve roots that exit the cervical spine is being compressed. The symptoms that occur could relate to the level at which nerve compression is occurring. This means that what aggravates symptoms may be different for every person. Some potential triggers include posture in which the head tilts forward or down, strenuous activities, and sleep position.
Can Cervical Stenosis get better on its own?
There is no cure for cervical stenosis because it is often caused by wear and tear and the natural degeneration of the spinal structure. That said, most cases of stenosis respond well to nonsurgical treatment. The typical plan of care for spinal stenosis includes injections and physical therapy as forms of symptom management before surgery is considered.
How is it treated?
When medication and physical therapy do not provide a sufficient degree of relief from symptoms of cervical spinal stenosis, a specialist may recommend surgical intervention. Cervical foraminotomy is a common procedure performed to improve comfort and range of motion.

The foraminotomy procedure widens the portion of the spine where stenosis has occurred. This opens up space for nerve roots to exit the spine normally, without compression. The procedure involves a small incision in the neck, through which the surgeon can access the affected vertebra. Here, blockages such as bone spurs may be removed and the spinal canal widened through adjustments to the intervertebral foramen. Spinal decompression and fusion may be performed if needed to fortify the structure of the spinal column in the cervical area.
How can I prepare for Cervical Spinal Stenosis treatment?
The doctor may order imaging or other tests to be evaluated before surgery. This can help with the treatment planning process. Patients can also expect to receive detailed pre-operative instructions that will advise them regarding medications and supplements to avoid. During the consultation, it is important to discuss all prescription and nonprescription medications that are taken, including vitamins and supplements. Part of preparation for surgery is to reduce the risks of bleeding, which may stem from certain products. Patients who smoke need to refrain from tobacco use of all kinds beginning two weeks before surgery.
Is it painful?
The foraminotomy procedure is performed using general anesthesia. Patients are in a sleep state, in which pain receptors in the brain do not receive signals from the body. No pain is experienced, and patients have no memory of their procedure. While under general anesthesia, patients are under the close observation of a board-certified anesthesiologist who monitors their vital signs. The surgeon utilizes x-ray imaging to visualize the exact location where the foramen requires widening.
After surgery, patients may feel sore or tender. The surgeon may prescribe pain medication that should be taken as directed for a few days.
What is recovery like?
Patients are usually back home within 24 hours of their procedure. Post-operative instructions are provided and are usually in effect for about six weeks. These may include:

- Cervical collar. This may be soft or somewhat rigid. The purpose of wearing the cervical collar is to limit movement that could cause discomfort.
- Activity restrictions. Patients must avoid strenuous activities, repetitive motions, and heavy lifting for six weeks following surgery. They may also need to avoid driving until they can resume this activity safely with full ability to view blind spots.
- Walking. Walking is the primary post-operative physical activity recommended for all patients. It helps with blood circulation and minimizes the chances of blood clots in the legs stemming from inactivity. It is important to take short walks several times a day.
Some patients may be able to return to work approximately two weeks after their procedure. Depending on the type of activities they must perform on the job, some may need to wait the full six weeks to recover before returning to work. At six weeks and possibly also at 12 months, follow-up x-rays may be taken to view the spine when flexed and extended.
Can Cervical Spinal Stenosis flare up again after treatment?
It is impossible to guarantee the long-term outcome of cervical foraminotomy for cervical spinal stenosis. However, studies indicate the instances of reoperation are less than 10%. Most patients experience an acceptable level of symptom improvement from their treatment. When you consult with one of our experienced providers, you can expect a comprehensive examination and discussion regarding the potential and expected improvements that surgical intervention may achieve in your case.
Schedule Your Consultation Today!
Questions? Please call us at 214-823-2052 to book a consultation with one of our providers today!