Our spinal discs are little shock absorbing miracle workers…until they’re not. They transform from excellent providers of cushioning to bulging, herniating objects that, when they begin to push on surrounding nerve structures, can be the cause of back pain.
So, what’s the process of this happening? There is a term used in some circles to describe the process, the “degenerative cascade.” Since our neurosurgeons deal with the aftermath of this process every day with our Texas Neurosurgery patients, let’s get into that process in this late fall blog.
The progression
When we’re born that could be the only time in our life that our spinal discs are relatively normal, at least in the sense of fulfilling their function. They’re full of water, they’re normal in shape, they’re normal width, and they provide all the cushioning and allow all the painless movement that are hallmarks of youth.
Then they start to change. Most researchers believe what happens is the chemicals inside the disc change. These chemicals are called proteoglycans, and their makeup changes and this doesn’t allow the disc to hold the same amount of water in the center of the disc as it did when we were young. The water begins to seep out of the disc. When water begins to leave the disc that’s when discs change. They herniate, bulge, thin, and become far less cushioning. They harden.
The stages of degeneration
In the 1970s, William Kirkaldy-Willis described the degenerative cascade. This model helped to explain the normal changes that all spinal discs go through. He believed that after a torsional (twisting) injury to the disc, the degenerating disc follows these three general stages:
- Dysfunction — Small circumferential tears in the outer layer of the disc grow inward. After injury, mobility may be limited.
- Relative instability — Inner material of the disc begins to protrude outward through the tears, leading to decreased disc height.
- Restabilization — Osteophytes form at the margins of the disc and the changes in the disc become fixed. The vertebral segment restabilizes and dysfunction subsides.
The stages of degeneration may occur over a period of two to three decades, with pain less likely and less frequent in older age. Adults over 60 years old are less likely to have pain from degenerative discs than adults between 30 and 50 years old. Pain from other degenerative conditions, such as degenerative osteoarthritis or spinal stenosis, is far more likely in elderly adults than pain from degenerative disc disease.
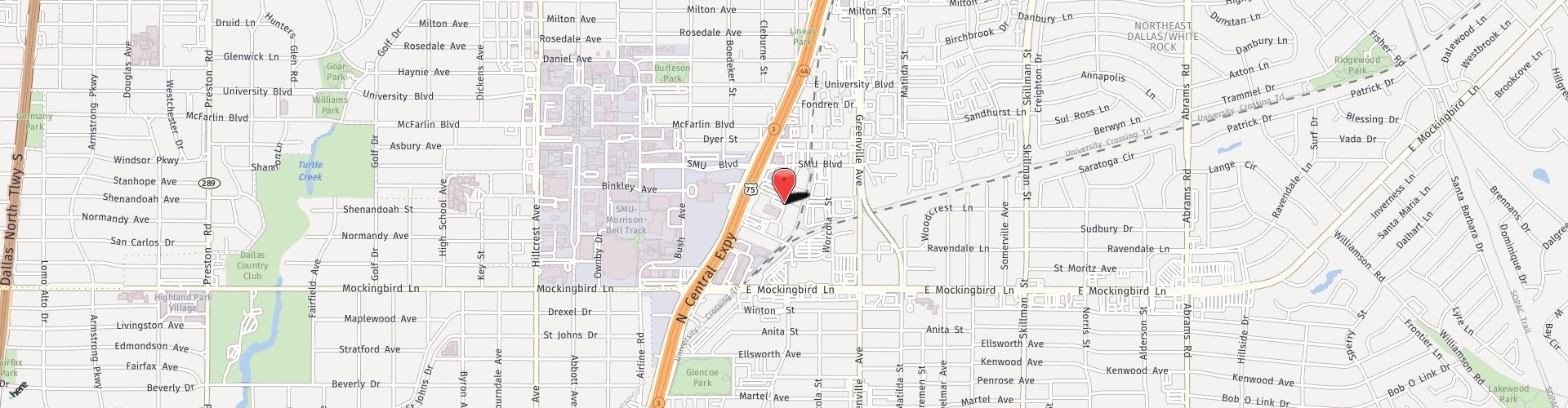
Do you have chronic back pain? It’s time to give our experienced team at Texas Neurosurgery a call at (214) 823-2052 to schedule an appointment.